Nothing over the past decade has been more demonized than this item. Everyone from Harvard researchers to the front desk clerk at your local grocery store knows about it. It’s some of the most generic health advice you can receive: “Oh you have X problem, just stop eating gluten.” “You have Y symptoms, have you tried cutting gluten out of your diet?” Even some healthcare practitioners will advise their patients, “Oh you have an autoimmune disease, you can never eat gluten again.” It’s these sorts of fear-mongering tactics that leave people afraid of food, afraid to go out with friends because there might be some gluten in the salad dressing, and afraid to have a piece of cake at their child’s birthday party. It can consume so much of one’s life, almost to the point where your health starts to suffer at the expense of pursuing what you think is healthy, not eating gluten.
Hashimoto’s thyroiditis is one of these autoimmune conditions that is brought up quite frequently in regards to avoiding gluten consumption. Hashimoto’s is an autoimmune condition where your immune system starts attacking your thyroid gland, thinking it’s a foreign invader. For some, the thyroid can become so damaged that it no longer produces optimal levels of thyroid hormone, while others are able to get control of their autoimmunity before it gets that severe. Lifestyle, and diet particularly, has a huge role in how your autoimmunity plays out, but what do we know about the role gluten plays in Hashimoto’s? Will cutting it out for a few weeks be enough? Or do I need to be gluten-free forever? What is it about gluten that can be so problematic for those with Hashimoto’s?
Gluten’s Potential Role in Hashimoto’s
Gluten is a protein found in wheat, barley, and rye. Proteins are made up of a particular combination of 20 different amino acids. In other words, you need to bond amino acids together in order to make proteins. Our thyroid gland is also made up of amino acids and proteins. For some people, eating gluten causes an inflammatory response, basically the immune system’s version of saying “Hey we don’t like this protein so we might have to attack it.” What the immune system could be attacking specifically is the amino acid sequence of gluten (A-T-P-L). Parts of our thyroid gland look very similar to this amino acid sequence (A-L-P-L). The only thing that’s different is one letter, one amino acid. Our immune system sees this as “close enough” and decides to attack everything that looks like gluten when we eat it. Sorry thyroid gland, you look a lot like gluten.
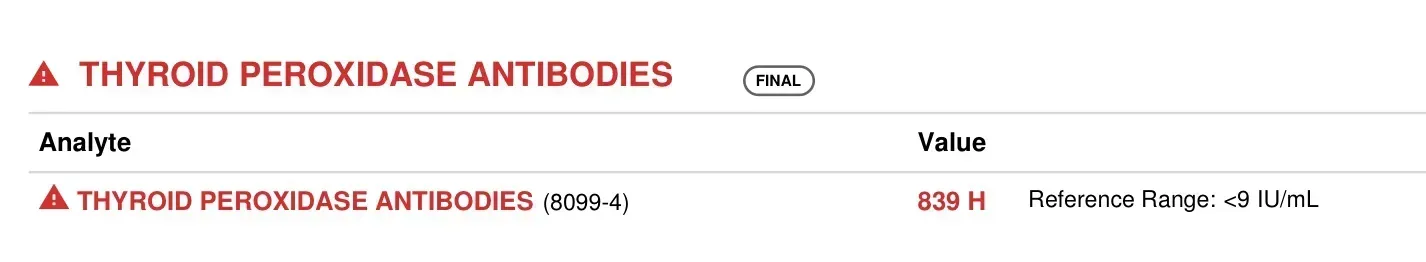
Researchers examined a part of wheat known as Wheat-Germ Agglutinin (WGA), and measured the immune response to WGA. They found that antibodies to WGA had “strong reactions…with TPO” (1). TPO (thyroid peroxidase) is an enzyme in the thyroid gland that helps with the production of thyroid hormones. If you have Hashimoto’s, you’ve likely had your TPO antibodies tested to help confirm the diagnosis (see image below).