Weight loss struggles, dry skin, and fatigue may lead you to believe that you have a “thyroid problem”. You go to your physician, tell them your complaints, and have some thyroid labs done. “Once these labs come back, I’ll know what’s wrong with me” is what you’re telling yourself. Several days later, your physician calls you, and you hear the last thing you wanted: “Your labs are normal.” The first thing you’re thinking is “how on earth are they normal?! I feel terrible!”
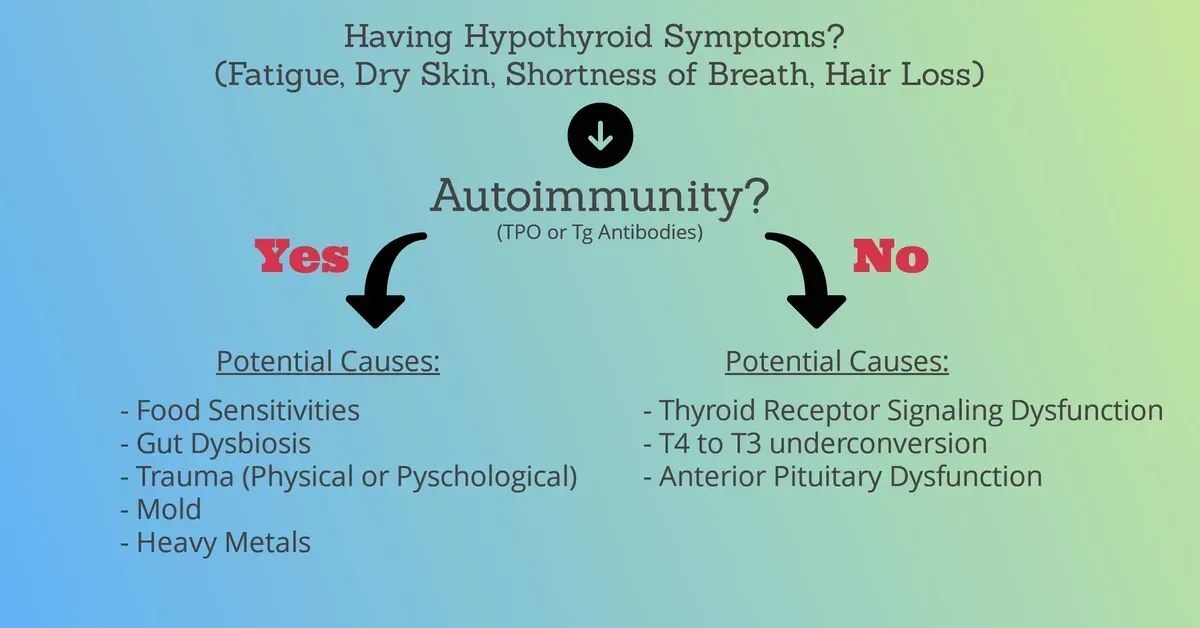
The issue with some of the thyroid symptoms, such as fatigue, constipation, brain fog, is that they are vague symptoms that could really be caused by anything. While yes, your thyroid may not be functioning optimally, the cause of this dysfunction may be coming from somewhere else. There’s nothing inherently wrong with the thyroid itself, but maybe there’s some dysbiosis in the microbiome, maybe you’re not properly digesting and absorbing your food, or maybe you’re under high amounts of stress at work. All of which just happen to be manifesting as “thyroid” symptoms.
If you’ve been to any functional/national/integrative practitioner, they’ve likely mentioned the concept of “functional ranges” with you. Personally, I prefer the phrase optimal ranges. The idea is that the standard medical ranges are too wide, and your levels should be within a more narrow, functional range. This conversation deserves its own article, and there is lots of controversy on what “optimal” lab ranges are. This leads us into what tests we have for assessing thyroid function (Check out that article if you want to take a deeper dive into thyroid lab tests).
It Must Be My Hormones
T4 and T3 are the actual “thyroid” hormones. From there we can specify the quantity of free versus bound T3 and T4. Free means the amount that’s ready for our cells to use. T4 is the most commonly produced hormone (80–90%), while T3 is the active hormone, meaning it’s this form that our cells can actually use. Why on earth would the body produce large amounts of something it doesn’t actually use? Pure speculation here, but I think it’s a survival mechanism.
Whenever your body wants to conserve energy during a state of “trauma”, such as during an automobile accident or an acute illness, the body has less demand for thyroid hormone. Therefore, the body won’t convert as much T4 to T3, but rather, T4 will be converted to reverse T3, an inactive alternative to T3. There are blood tests for reverse T3. Unfortunately, there isn’t much data to say it’s clinically meaningful (1).
You can very easily have normal thyroid hormone levels and still feel terrible. I’ve seen it many times with patients who are on thyroid hormone therapy. Their levels are back in the “normal” range since getting on medication, yet they feel no difference. Again, this is because the root cause is coming from somewhere else.
Most Common Cause of Hypothyroidism
You might have thyroid autoimmunity (Hashimoto’s). Many physicians, when checking your thyroid function, will only run TSH (Thyroid Stimulating Hormone). While this may be a decent marker for T4 and T3 status, it does not account for 90% of the causes of hypothyroidism in the US, autoimmunity. If you have autoimmunity, your immune system could literally be attacking and reducing the functional capacity of your thyroid gland, kind of like a tornado physically destroying the kitchen of a restaurant. It’s probably not a functioning restaurant anymore.
Knowing whether you have autoimmunity or not should completely change the treatment approach. If you do, a clinician should conduct a thorough history to identify the root cause of your autoimmunity, aka what started it. As discussed above, this can come from gut dysbiosis, improper stress management, or even heavy metals.